Tinnitus basically means – unpleasant buzzing or ringing in one’s ears. But, despite being a bit annoying, it sounds harmless, right?
In reality, tinnitus should be treated very seriously especially because it is not a disease per se; it is a symptom of an underlying condition. In some cases, it can suggest that there is a tumor on a vestibular nerve or in a brain tissue. When this unpleasant symptom occurs make sure to contact your doctor for further diagnostics.
An increasing number of researches established a connection between blood pressure disturbances and tinnitus. Find out more about this condition, and how the blood pressure affects it.
Blood Pressure—Definition and Disorders
Blood pressure is defined as the force of blood pushing the blood vessels. It has two components—systolic (pressure when the heart beats) and diastolic (pressure when the heart rests). The normal blood pressure for adults is the systolic pressure below 120 mmHg, and diastolic pressure below 80 mmHg. Higher or lower values do not necessarily mean that the person is ill. Some activities such as running or even stress can cause elevated blood pressure. On the other hand, consumption of certain foods, for instance garlic, can cause lowered blood pressure.
When it comes to high blood pressure or hypertension, as a condition it can be dangerous for one’s health, and even fatal. It can cause heart attack, stroke, peripheral artery disease, eye disease, etc. Low blood pressure (hypotension) can be responsible for fatigue, dizziness, lightheadedness, fainting, vision impairment, confusion, nausea.
Digital Health
The convergence of digital technology with health is rapidly and confidently taking its steps to the future. Digital health area focuses on improving outcomes by making information for efficient patient monitoring in hospitals, disease management or it can simply serve as a proactive preventive care. Digital technology also found its application in blood pressure monitoring.
It is easy to conclude that blood pressure control is important. The higher it is the higher is the risk of developing health problems in the future. To avoid any future complications, every household should have a blood pressure monitor. Choosing the right one is not an easy task, since there is a whole variety available on the market.
The basic types of home blood pressure monitors come in arm-cuff and wrist-cuff models. The principal is the same – the cuff is inflated to temporarily cut off blood supply. The cuff is subsequently released ant the point at which blood begins to intermittently flow is sensed. This is the systolic pressure. The diastolic pressure is detected when the flow goes from an intermittent to continuous flow.
Arm monitors automatically inflate the cuff and display the readings. Some models offer the option to download results to a computer, making the data easy to share with your doctor. Multiple user memories allow more than one person in your household to monitor and record their blood pressure.
Wrist monitors are fully automatic, compact, lightweight and portable. The only flaw is their sensitivity to body position.
The latest digital techniques produced upper arm blood pressure monitors. Its simple to use one-touch measurement allows the user to get precise data of their heart’s health. Many modern blood pressure monitors have varying features, storage capacity and smartphone connectivity.
One other digital innovation is the opportunity to combine blood pressure monitor and blood pressure calculator. This tool enables you to find out whether your blood pressure is low, normal or high. It is very simple to use. You just have to input your systolic and diastolic blood pressure values into the tool (mmHg). The app immediately calculates your average blood pressure. In addition, there is a chart on average blood pressure by age, so you can compare your values to those in the chart.
Doctor’s advice is, however, always the primary guidance.
What is tinnitus?
Do you suffer from ringing in your ears or noises in your head? If so, it doesn’t mean you are going crazy. You may be suffering from a condition perceived by one in ten adults, called tinnitus (lat. tinnire – to ring). According to Roberts et al., tinnitus can be described as – conscious perception of a sound that is not generated by any source outside the body. Besides ringing and buzzing, these sounds are sometimes more complex, fluctuate over time, and can be perceived in one or both ears or be heard diffusely in the head.
Is There a Connection Between Tinnitus and Blood Pressure?
There are some studies about hypertension in patients with tinnitus which suggest the existence of a connection between these two conditions – Novak et al.’s study on “Tinnitus in systemic diseases”, included 1200 patients treated form tinnitus, and 47% of them suffered from hypertension. Sogebi’’s study – “Characterisation of tinnitus in Nigeria” (2013) showed that 15.2% of the 79 patients suffering from tinnitus were also suffering from high blood pressure. Research conducted on the Positive Association between Tinnitus and Arterial Hypertension analyzed the presence of arterial hypertension in tinnitus and non-tinnitus patients. Based on the sample of 144 patients in the tinnitus group and 140 in the control group, an association between tinnitus and arterial hypertension was established.
The pathophysiological mechanisms of tinnitus are still unclear. Abnormal blood flow through the blood vessels in the brain may cause tinnitus. According to “The Handbook of Tinnitus” (Adrian, D. and El Rafaie, A., 2000), this can subsequently, lead to an increased spontaneous firing rate of neurons in the central auditory system of the brain and the overall reorganization in the auditory modality.
Some animal experiments indicated that high blood pressure has the ability to cause damage to cochlear microcirculation. To be more accurate, stria vascularis, which feeds the organ of Corti, suffers the highest impact. Przewoźny et al.’s study revealed that this can lead to a decrease in the oxygen partial pressure in the cochlea, and the disturbance of the ionic K+ recycling.
Additionally, some blood pressure medications can cause tinnitus. Antihypertensive drugs can cause an adverse effect by damaging the patient’s labyrinth.
Low blood pressure or hypotension can also cause a similar sensation due to insuficient blood flow to the brain, which might result in buzzing in the ears, dizziness, and lightheadedness.
Conclusion
To sum up, tinnitus can be caused by many serious conditions, such as brain tumor, atherosclerosis, neck injury, vestibular nerve damage, high or low blood pressure, and even blood pressure medications. As a symptom, especially if it occurs only in one ear, it can point to a tumor on a vestibular nerve and it should not be taken lightly. Next time you experience this annoying ringing, don’t delay your visit to the doctor – it just may save your life!
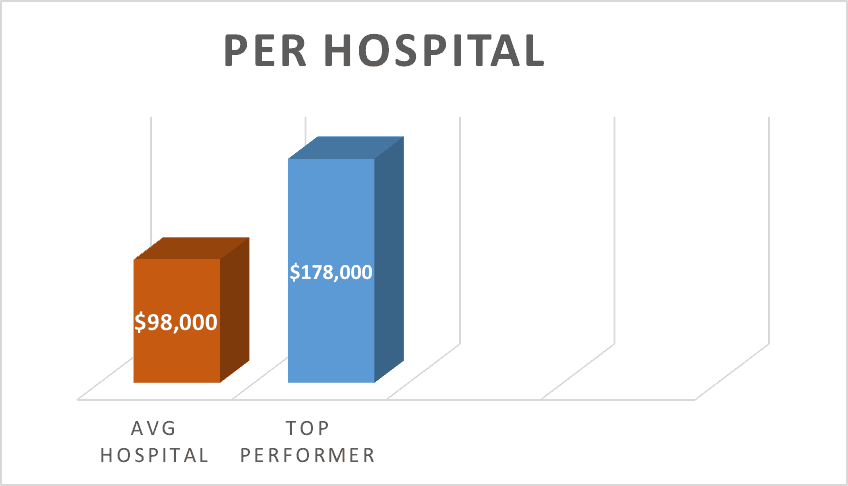
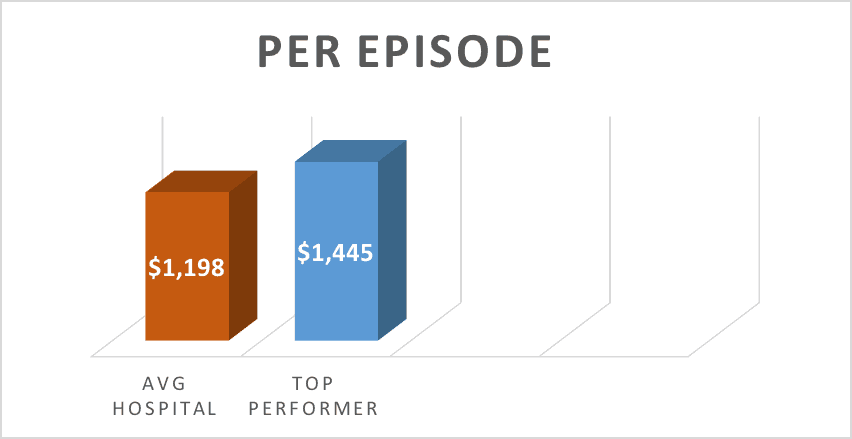
 Existing digital health products, if deployed comprehensively across the country, could save the US $7 billion a year in healthcare spending, according to
Existing digital health products, if deployed comprehensively across the country, could save the US $7 billion a year in healthcare spending, according to